Frontal and temporal lobe dysfunction in autism and other related disorders: ADHD and OCD
Michael Goldberg1, Ismael Mena1, Bruce Miller1.1 - Clínica Las Condes, Santiago,Chile, Dept of Neurology, UCSF Medical Center..
Summary
Autism, Pervasive Development Disorder (PDD), Attention Deficit Hyperactive Disorder (ADHD), and Obsessive and Compulsive Disorder (OCD) involve significant frontal and temporal lobe dysfunction. This conclusion is based on NeuroSPECT work now in progress on children afflicted with these disorders. We have been using NeuroSPECT to image cerebral abnormalities of perfusion/function in Autism, ADHD, OCD, and other neuro-cognitive disorders.
With the increased focus and presentation of children labeled Autistic Syndrome / PDD, has come a greater need to understand and define the dysfunction in these children by objective "functional" quantification, now possible with new imaging technology such as NeuroSPECT.
The children have been evaluated by means of Xe133 for SPECT, expressing the results three-dimensionally and rCBF quantitatively in ml/min/100g; and qualitatively by means of Tc-99 HMPAO. The correlation of cerebral perfusion with brain function has been established, as NeuroSPECT is a useful tool for cerebral function assessment.
In this review paper, we will discuss our clinical observation and our rCBF findings for Autism and these related disorders.
The new definition of autism
Autism as classically defined was a severely incapacitating disability that was relatively rare. Its onset was in early childhood. This disorder was characterized by delays in language development, marked social deficits and a limited range of stereotyped repetitive behaviors. It occurred in approximately 1-2 out of every 10,000 births. Boys were afflicted more frequently than girls at a 3:1 ratio.
In this severe form of "Classic Autism" effective speech was absent. It could include symptoms of repetitive, highly unusual, aggressive and self-injurious behavior. Those afflicted had extremely abnormal ways of relating to people, objects, or events. Parents noticed that something was "not right" in the first three to six months of life.
Autistic infants did not demand attention, they did not enjoy being picked up, nor did they cuddle or cling when someone held them. They rarely smiled at other people or looked directly at them. In fact, they often appeared happiest when left alone. They resisted affection and did not interact normally. Mothers of autistic children often noted an understandable lessened pleasure in their maternal efforts. They complained that they felt they were caring for an "object" rather than a person.
In the last decade, another type of autism has surfaced that is often referred to as "Autistic Syndrome." Children suffering from this disorder appear normal in the first 15-18 months of life. They do not present signs or symptoms pediatricians or neurologists would find atypical. These children create an inconsistency with previous held beliefs that 70-80% of autistic children are mentally retarded. They crawl, sit up, walk, and usually hit normal motor milestones on schedule. Up until the age of onset, they are affectionate and appear to have above average intelligence.
Children with autistic syndrome may begin to develop some speech but then, without warning, they cease to progress, or begin to regress. Suddenly, these children become withdrawn. They are quiet sometimes and hyper at other times. Often self-stimulatory behaviors (i.e. arm flapping, rocking, spinning, or head banging) develop.
These children begin to display various abnormal behaviors in the preschool years often including:
- A need to preserve sameness
- Marked language abnormalities
- Indexes of developmental disorder - strange body movements, posturing and "soft" signs of neurological impairment
In time, some manifest symptoms that are both similar and atypical to children previously diagnosed as "classically autistic." What was once a relatively rare disorder is now twenty times more likely to occur.
In the past, autism was considered a "psychiatric" disorder. We now know that autism is a "medical condition," not a mental disorder. Perhaps one of the reasons no one has come up with an answer for autism is the way we have thought of it (or rather did not think of it in medicine).
Most researchers did not look for the answers to autism because they felt this was a disorder that was untreatable medically. Treatment for this affliction was primarily left in the hands of psychologists and a few psychiatrists.
Even though children with classic autism might be helped medically as our knowledge of the brain’s physiology expands, for now it might be helpful to separate children afflicted with autistic syndrome from those with classic autism. As children with autistic syndrome increasingly become categorized as a "medical" problem, separating them from the many negative connotations and hopelessness associated with "classic" autism could be advantageous to promoting research and funding to help these children. The differences between the two groups may be summarized as follows:
Classic Autism
- A rare disorder affecting 1-2 children / 10,000
- Some/many individuals may have early signs of neurologic injury
- Some may have "physiologic/immune" factors / variables, "treatable" medically by current and future immune medicines
- Generally "abnormal" early (i.e. 3 - 6 months of age)
- "Classic" Autistic symptoms / presentation
- Presumed "static" / unchangeable
Autistic Syndrome
- An increasing population of children with "Autistic/ PDD" behavioral characteristics.
- Atypical symptoms
- Asperger’s
- Landau Kleffner’s
- ADHD / ADD variant
- Current estimate 20-40 children / 10,000 (incidence may be as high as 1-5%)
- Does NOT have "objective" physical signs of neurologic damage
- Majority (possibly all) are immune mediated, appropriately looked upon as a medical dysfunction - open to potential medical therapy
- Generally "normal" early (usually until 15 - 18 months of age)
- Potentially progressive disorder (if not treated / corrected) which may explain the origin of many cases of Landau-Kleffner syndrome
Etiology
While the cause of autism is speculative, different theories that have surfaced in the past include:
- Brain injury
- Constitutional vulnerability
- Developmental aphasia
- Deficits in the reticular activating system
- An unfortunate interplay between psychogenic and neurodevelopmental factors
- Structural cerebellar changes
With the relatively new thinking that autism has medical origins have come several other theories. Some doctors believe autism is a result of a metabolic, enzyme, or genetic defect. Although a few children may suffer a built-in genetic or functional defect present since early gestation, our clinical observation and our rCBF findings for Autism do not support these theories for the majority of children afflicted. These theories do not fit or began to explain the large increase in the number of children diagnosed with autism today.
Research to support immune dysfunction theory
Similarities between behavioral deficits reported in animals with hippocampal lesions and autistic behavior have been noted by Boucher and Warrington(1). They found memory deficits in infantile autism similar to the memory deficits found in the amnestic syndrome. Medial temporal lobe damage on pneumoencephalograms has previously been reported in a subset of autistic children(2). These findings were particularly evident on the left side. Damasio and Mauer have also proposed that "the syndrome results from dysfunction in a system of bilateral neural structures that includes the ring of mesolimbic cortex located in the mesial frontal and temporal lobes, the neostriatum, and the anterior and medial nuclear groups of the thalamus." (Noteworthy, is that much emphasis is put on the medial temporal lobe).
By definition, autism has an early onset before 30 months of age, while disorders appearing later in life have been thought to be symptomatically different from autistic handicap conditions. Publications over the last 13 years have cast some doubt on these relationships. It has been pointed out that there is no firm evidence that similar or identical syndromes might not develop in older children(3).
Autism can be associated with a variety of disorders affecting the central nervous system including encephalitis. In 1981, DeLong, Bean, and Brown described three children between 5 and 11 years of age who developed autistic features while having an encephalitic illness. One patient had high serum herpes simplex titers, and a CT scan revealing a lesion of the temporal lobes, mainly on the left side. The other two patients had normal CT scans.
Gillberg in 1986 described the case of a 14-year old girl who developed a "typical" autistic syndrome after an attack of herpes simplex encephalitis(4). Widespread bilateral destruction of the brain parenchyma and the temporal lobes was found on CT; there was also some involvement of the lower parts of the parietal lobes. The autistic symptoms persisted long after the acute phase of the encephalitic illness.
In 1975 an article was published in Cortex(5) describing a syndrome similar to autism in adult psychiatry, involving loss of emotional significance of objects, inability to adopt in social relationships, loss of recognition of the significance of persons, and absence of sustained purposeful activity after temporal lobe damage.
In 1989 an article appeared in the Journal of Autism and Developmental Disorders(6), describing a 14-year old boy, with a normal history until the second grade, when he was admitted to the hospital with herpes simplex encephalitis. Later he developed significant language, social, and memory deficits. The research group commented on the cognitive and behavioral deficits caused by temporal lobe damage in herpes encephalitis. While other studies have also implicated the temporal lobes in the pathogenesis of autism(7,8) this does not prove a common association between temporal lobe pathology and autism. Research has found a variety of lesions in the brain, particularly the cerebellum(9) since Herpes virus has a predilection for the temporal lobes(10) it is possible to hypothesize that there is an association between temporal lobes and autism, but not necessarily a direct cause and effect relationship(11). It is equally important to note that failure of development in temporal lobes early in life may produce different symptoms from those arising out of a later destruction of previously normal lobes.
From the Journal of Clinical Immunology and Immunopathology, Singh et al. hypothesized that autoimmunity secondary to a virus infection may best explain autism in some children(12). Congenital rubella virus(13) and congenital cytomegalovirus(14) have been indirectly involved as causative factors in autism. Researchers found evidence for autoimmunity as a possible mechanism to explain autism, based on a cellular immune response to myelin basic protein(15), antibodies against putative brain serotonin receptors(16), and neuron-axon filament proteins of the nerve cell(17).
Autism and the Immune System
It is our belief that "Autistic Syndrome" probably is a state of dysfunction induced in the brain by a dysregulated immune system. It is possible that this dysfunction may occur in individuals that have a genetic predisposition. In theory, this predisposition could be triggered by various stresses placed on the child’s immune system. It’s severity varies with the individual and age of onset.
It can be compared to blindness. There are many people who are blind, but the cause of their blindness may be very different. For whatever the reasons (genetic, environmental, a combination of viruses, etc.), what is occurring appears to be an immune mediated, abnormal "shut down" of blood flow in the brain and therefore central nervous system function.
In adolescents and adults, this dysfunction may manifest itself as CFIDS (Chronic Fatigue Immune Dysfunction Syndrome), ADHD, and various other atypical auto-immune disorders associated with neuro-immune dysfunction. In older children, it is seen as variants of ADD (Attention Deficit Disorder) / ADHD. And in younger children/infants, it appears as autism, autistic syndrome and PDD (Pervasive Development Disorder).
The multiple metabolic, physiologic, and immune markers that are abnormal in these children, "make sense" when you think of the bigger picture and consider the primary cause of autism as immune dysfunction, creating multiple cellular / mitochondrial dysfunctions.
This offers an explanation for the progressive process of the autistic syndrome that occurs sometime between 15-24 months of age. It is this immune mediated, abnormal "shut down" of blood flow in the brain that affect the language and social skills area of the brain and central nervous system function.
Clinical Manifestations
Typical characteristics include:
- nondeveloped or poorly developed verbal and nonverbal communication skills
- abnormalities in speech patterns
- impaired ability to sustain a conversation
- abnormal social play
- lack of empathy
- an inability to make friends
Also frequent seen are:
- stereotypic body movements
- a marked need for sameness
- very narrow interests
- preoccupation with parts of the body
- change of hand or becomes ambidextrous, as they turn autistic.
-
With several different etiologies or biological causes, autism is considered a syndrome rather than a disease. Some researchers have proposed genetic defects(18), viruses(19,20) and immunological ties(21,22,23) to be the cause.
While the literature has speculated regarding the above hypothesis and many others, at this time there appears to be an enlarging group of children, whose origin seems linked to the concept of an Immune-Dysregulatory phenomenon. The dysfunction / lack of blood flow can eventually lead to injury of nerve cells, which offers a possible explanation for the abnormal brain waves and the large numbers of autistic syndrome children suddenly being labeled as "Landau-Kleffner."
Whether due to an underlying viral, retro-viral, or other related entity, a likely underlying genetic disposition, and/or other "environmental"factors, the number of children affected seems to be rapidly increasing. Many of these children do not fit classic autistic profiles, but are frequently labeled high functioning autistic, atypical autistic, PDD, etc.
NeuroSPECT Results
Quantitative rCBF measurements with Xenon 133 were found to be significantly higher than normal in autistic children, with maximal values in the frontal lobes and visual cortex. Minimal perfusion was observed in the temporal lobes. Decreased flow was also noted in the cerebellum and occipital lobes.
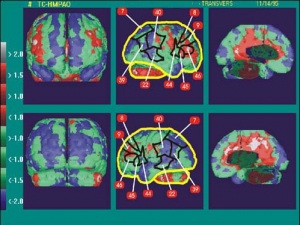
The areas of increased perfusion, most frequently located in lateral frontal lobes, are similar to our observations in obsessive compulsive disorder (OCD children). Tc 99m HMPAO images (Prado et al.) demonstrate increased frontal perfusion, and demonstrating also temporal, occipital and cerebellar hypoperfusion. (Figure 1)

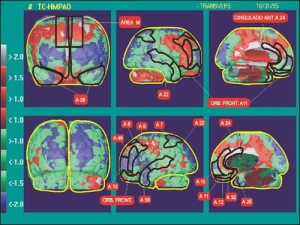
In children with OCD there is a significant increase in frontal perfusion observed bilaterally in a large number (~ 81%) of the children and unilaterally in a limited number (6%) of the children, with a total of 87% of children demonstrating increased frontal perfusion. Among 50% of these children there is also increased perfusion in the posterior cingulate gyrus. Of note, there is furthermore hypoperfusion of temporal lobes mostly in the mesial aspects in 93% of OCD children examined to date.( Mena et al)
Increased frontal perfusion was also reported (Rubin et al.) in adults. Most probably this phenomenon denotes a co-morbidity phenomenon also that is clinically observed between autism and obsessive compulsive disorder.
Discussion of NeuroSPECT Results
NeuroSPECT scans are becoming extremely informative, as they show blood flow through areas of the brain. Blood flow implies function / activity(24,25). As noted, the autistic children have presented consistently with a decrease in blood flow in the temporal area, various degrees of hypoperfusion in the parietal / occipital area and the cerebellum vermis. There has often been an increase of blood flow in the frontal lobes which is consistent with ADD on the hyperactivity end. Figure 2.
The clinical implications of these findings has been heightened by the fact that the "anatomic" areas of the brain involved on the NeuroSPECT have correlated with predicted areas of dysfunction when reviewed by neuro-anatomists (research work in progress). In fact, the areas of dysfunction on Neuro-SPECT, have helped explain readily the physiologic dysfunction of these children.
These children present with a symptomatology consisting primarily of severe speech and language development (Left temporal lobe) and severe social difficulties (Right temporal lobe), often some fine, not usually gross, motor difficulties (cerebellar involvement), and various learning difficulties and attention deficit dysfunctions consistent with involvement of frontal and temporal lobes, and links to areas of parietal-occipital dysfunction. They may also have many symptoms consistent with OCD characteristics, associated with these areas of dysfunction.
In 1995, Mountz, Tolbert, Lill, Katholi and Liu reported their HMPAO findings in 6 children with severe autism and demonstrated with semi-quantitative techniques temporal and parietal hypoperfusion with lateralization to the left hemisphere, while in two of the three images published there is a maximal perfusion in the lateral frontal lobes.
Georges, Costa, Coniz, Ring and Ell reported in four autistic adults with Tc-99 HMPAO diminished rCBF in temporal and frontal lobes. The temporal abnormality appears to be confirmed mostly in adults, adolescents, and children suffering of autism. Thus, damage to temporal lobe in an early developmental stage may result in autistic manifestations.
The results are otherwise heterogeneous translating the heterogeneity of the autistic population, denoting the presence of occipital hypoperfusion and cerebellar hypoperfusion mostly in the mesial aspects corresponding to the vermis area. This later observation correlates with reports in the literature of atrophy of the cerebellar vermis demonstrated by MRI technique. Further heterogeneity in our group of patients is demonstrated by apparent comorbidity with OCD (and ADHD) in these children and their typical presentation of increased perfusion in lateral frontal lobes. (figure 3)
Discussion
Autistic children are an heterogeneous group. Increased frontal perfusion may be related to "hyperfrontality" disorder, and cerebellar hypoperfusion to motility impairment. Temporal lobe hypoperfusion and other areas of dysfunction remains in spite of multiple various therapies used by these children. We are looking at anatomical markings, defining autism / PDD dysfunction, correlating to models proposed by behavioral neurologists.
Past focus for autistic children has been on trainability, cooperation, behavior, NOT on improving the cognitive processing. A shift to the idea of "rehabilitation" is already in motion, a full review of techniques and goals is urgently needed.
Based on NeuroSPECT findings, implications are that medications or efforts to "calm" the brain and child down, may further shut down the areas in which we want to improve blood flow and function and down regulated blood flow.
Clinical experience to date has noted with medical intervention to help normalize their dysregulated immune systems many of these children up to 5 or 6 years of age will often "turn-on" and pick-up where they stopped, generally about 18 - 24 months old. On the other hand, as children approximately 6 - 10 or 11 years improvement is a slower process, often requiring more "help" to "learn" the basics, grow-up developmentally, and then move ahead successfully.
For most children, it will probably take the advent and usage of new drugs that are immune modulators, to truly shut off their dysregulated immune system. Although these drugs are already in existence and are now undergoing new usage testing in adults, they still await testing for children. Hopefully, they will have the ability to adjust the dysregulated function and put the immune system back on track. The clinical implications and concepts related to past hypotheses of brain develop and maturity, are intriguing to say the least.
It was and still is believed by noted neurologists that nothing can be done medically to treat these children. Fortunately, as these children are changing with therapy, respected neurologists and other pediatric researchers, are beginning to feel it is time to "take a second look."
The good news is that children afflicted with autism whose immune systems have been helped are showing they are bright thinking individuals who are not what the world expected. Children with the "label" of Autism / PDD usually are not retarded. They may have normal or above normal intelligence. They are not throw away kids that cannot be helped. They are children who are suffering from temporal hypoperfusion / hypofunction, likely auto-immune mediated dysfunction, that can possibly recover.
While identifying and looking at different neurotransmitters, neuroscientists have also found different problems with too much or too little of one or the other. In people with too much norepinephrine everything is pumped up; every stimulation demands a response. The other side of the coin is that a shortage of norepinephrine seems to rob people of the ability to know what’s important. Working memory (the part that stores information while the mind considers if it is worth keeping and where to file it) fails without enough dopamine. Altered central dopaminergic function in the midbrain has been implicated in the pathogenesis of Tourette’s Syndrome. Finally, shortage of serotonin in the frontal lobes and in the brain’s limbic system seems to relate to impulsivity; obsessive-compulsive symptoms may be caused by a serotonergic defect involving the basal ganglia.
Conclusions
The observation of temporal hypoperfusion in adults and children with CFS / CFIDS, may define autism as a disorder of impaired relations with the surrounding environment determined by the temporal hypofunction leading as a consequence to a diaschetic hypofunction of visual cortex and cerebellum. The mechanisms for this abnormality need to be investigated using activation techniques and other approaches i.e. evaluation of possible immune dysregulation, etc.
With the general finding of a physiologic hypoperfusion / hypofunction on NeuroSPECT, with generally normal MRI’s and CAT scans, we are optimistically looking at areas of dysfunction amenable to therapy and improved return of function. Work is beginning (clinical research in progress) to define reasons for this function and in turn potential avenues of therapeutic intervention.
Referencias
- Boucher J, Warrington, "EK: Memory Deficits in Early Infantile Autism: Some Similarities to the Amnesic Syndrome," BR J Psychol 1976;67:76-87
- Hauser SL, DeLong GR, "Rosman NP: Pneumographic Findings in the Infantile Autism Syndrome: A Correlation with Temporal Lobe Disease" Brain 1975, 98:667-688
- Waterhouse, L., Fein, D., Nath, J., & Snyder, D. (1984), "Pervasive Schizophrenia Occurring in Childhood: A Review of Critical Commentary." In American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders(DSM-III): An interim appraisal. Washington, D.C.
- Gillberg, C.(1986), "Brief Report: Onset at Age 14 of a Typical Autistic Syndrome. A Case Report of a Girl with Herpes Simplex Encephalitis," Journal of Autism and Developmental Disorders, 16,369-375
- Marlowe,W. B., Namcall, E.L., & Thomas, J.J. (1975), "Complete Kl¸Ver-Bucy Syndrome in Man," Cortex 11, 53-59
- Greer,M K, Lyons-Crews, M., Mauldin, L.B. & Brown, F. R. III. (1989), "A Case Study of the Cognitive and Behavioral Deficits of Temporal Lobe Damage in Herpes Simplex Encephalitis," Journal of Autism and Developmental Disorders 19, 317-326
- Hetzler, B., & Griffin, J.(1981), "Infantile Autism and the Temporal Lobe of the Brain," Journal of Autism and Developmental Disorders 11, 317-330
- Jones, P.B., & Kerwin, R.W. (1990), "Left Temporal Lobe Damage in Asperger's Syndrome," British Journal of Psychiatry 156, 570-572
- Courchesne, E. (1991), "Neuroanatomic Imaging in Autism," Pediatrics 87(Suppl.part 2), 781-890
- Greer,M K, Lyons-Crews, M., Mauldin, L.B. & Brown, F. R. III. (1989), "A Case Study of the Cognitive and Behavioral Deficits of Temporal Lobe Damage in Herpes Simplex Encephalitis," Journal of Autism and Developmental Disorders 19, 317-326
- Ghaziuddin, M. Tsai, L.Y., Eilers, L. & Ghaziuddin N. "Brief Report: Autism anD Herpes Simplex Encephalitis," Journal of Autism and Developmental Disorders Vol. 22, No. 1,1992
- Singh V.K. , Warren R.P. Odell J.D. , and Cole P., "Changes of Soluble Interleukin - 2, Interleukin - 2 Receptor, T8 Antigen, and Interleukin - 1 in the Serum of Autistic Children," Clinical Immunology and Immunopathology 61, 448-455 (1991)
- Chess, S., "Autism in Children with Congenital Rubella," J. Autism Childhood Schizophrenia 1, 33-47, 1971
- Stubbs, E.G., Ash, E. and Williams, P.S., "Autism and Congenital Cytomegalovirus," J. Autism Dev. Disord. 14, 249-253, 1983
- Weizman, A. , Weizman, R., Szekely, G.A., Wijsenbeek, H., and Livni, E., "Abnormal Immune Response to Brain Tissue Antigen in the Syndrome of Autism," Am. J. Psychiatry 7, 1462-1465, 1982
- Todd, R. D., and Ciaranello, R. d., "Demonstration of Inter- and Intraspecies Differences in Serotonin Binding Sites by Antibodies from an Autistic Child," Proc. Natl. Acad. Sci. USA 82, 612-616,1985
- Singh, V.K., Fudenberg, H. H., Emerson, D. and Coleman, M., "Immunodiagnosis and Immunotherapy in Autistic Children," Ann. N. Y. Acad. Sci. 540, 602-604, 1988
- Folstein, S. & Rutter, M. (1977), "Genetic Influences and Infantile Autism," Nature, 265:726-728
- Chess, S.(1977),"Follow-up Report on Autism in Congenital Rubella," J. Autism Dev. Disord.,7:69-81
- Stubbs, E.G. (1978), "Autistic Symptom in a Child with Congenital Cytomegalovirus Infection," Journal of Autism- and Childhood Schizophrenia, 8:37-43
- Stubbs, E.G. (1976), "Autistic Children Exhibit Undetectable Hemagglutination-Inhibition Antibody Titers Despite Previous Rubella Vaccination," Journal of Autism and Childhood Schizophrenia, 6:269-274
- Stubbs, E.G.,Crawford, M. l., Burger, D.R. % Vanderbark, A.A. (1977), "Depressed Lymphocyte Responsiveness in Autistic Children," Journal of Autism and Childhood Schizophrenia, 7:49-55
- Warren, R. P., Stembridge, A. M. & Gardner, E.J. (1985), "Deficient Immune Function of Peripheral Blood Mononuclear Cells from Patients with Gardner Syndrome," Clin Exp. Immunol., 60:525-531
- Ichise M, Salit IE, Abbey SE, Chung D-G, Gray B, Kirsh JC, Freedman M. "Assessment of Regional Cerebral Perfusion in 99 Tem-HMPAO SPECT in Chronic Fatigue Syndrome," Nucl Med Comm 1992; 13: 767-772
- Costa DC, Brostoff J. Ell PJ. "Brain Stem Hypoperfusion in Patients with Myalgic Encephalomyelitis- Chronic Fatigue Syndrome (abstr.)" Eur J Nucl Med 1992: 19(8): 733
- Prado C.. and Mena I.. Basal and frontal activation neuroSPECT demonstrates functional brain changes in major depression. Alasbimn Journal1(3): April 1999. http://www.alasbimnjournal.cl/revistas/3/pradoia.htm
- Mena I., Sole,C.,Neubauer, S.,de la Barra,F., Garcia,R., Prado,C., Obsessive compulsive disorder in children: Spet of 99mTC HMPAO findings. World Congress of Nuclear Medicine, Berlín, 1998. European Journal of Nuclear Medicine 25:1077,1998
